Understanding Breast Augmentation
Breast augmentation, also known as augmentation mammoplasty, is a surgical procedure designed to increase breast size and enhance breast shape. This elective cosmetic surgery has become one of the most popular plastic surgery procedures worldwide, with hundreds of thousands of operations performed annually.
Women choose breast augmentation for various personal reasons. Some seek to restore breast volume lost after pregnancy, breastfeeding, or weight loss. Others aim to improve breast symmetry or achieve better proportioned figures. Many simply desire increased confidence in their appearance.
While the decision to undergo breast augmentation is deeply personal, understanding the complete process—from initial consultation to long-term maintenance—is essential for anyone considering this procedure.
Types of Breast Implants
Breast implants come in various types, each with distinct characteristics, benefits, and considerations. The main types include:
Saline Implants
Saline implants consist of a silicone outer shell filled with sterile salt water (saline). These implants are typically inserted empty and then filled once positioned, allowing for smaller incisions and some adjustment in size during surgery.
Advantages:
- If rupture occurs, the saline is safely absorbed by the body
- Ruptures are immediately noticeable as the breast size changes
- Often less expensive than silicone alternatives
- FDA-approved for women 18 and older
Disadvantages:
- May feel less natural, particularly in women with minimal breast tissue
- More likely to show rippling or wrinkling under the skin
- Slightly higher risk of cosmetic issues like visibility and palpability
Silicone Gel Implants
Silicone implants feature a silicone shell pre-filled with silicone gel, a thick, sticky fluid that closely mimics the feel of natural breast tissue.
Advantages:
- More natural look and feel compared to saline
- Less likely to wrinkle or ripple
- Better option for women with thin breast tissue
Disadvantages:
- Ruptures may be “silent” (not immediately apparent)
- Require regular MRI screenings to check implant integrity
- Typically more expensive than saline implants
- FDA-approved for women 22 and older
Highly Cohesive Gel Implants (“Gummy Bear”)
These newer-generation silicone implants contain a more cohesive gel that holds its shape even if the implant shell is broken.
Advantages:
- Maintain shape better than traditional silicone implants
- Lower risk of leakage if rupture occurs
- Reduced risk of rippling
- Available in anatomical (teardrop) shapes for a more natural breast profile
Disadvantages:
- Require longer incisions due to firmer material
- Usually the most expensive option
- Can rotate (if anatomical shape), causing breast distortion
Structured Implants
Structured implants combine elements of both saline and silicone technologies, using an internal structure to control the movement of saline within the implant.
Advantages:
- Natural feel with the safety profile of saline
- Reduced risk of rippling compared to traditional saline implants
Disadvantages:
- Limited long-term data compared to traditional options
- Not as widely available as saline or silicone
Implant Shapes and Sizes
Beyond the filling material, implants vary in shape, size, profile, and texture. These characteristics significantly impact the final aesthetic result.
Shapes
Round Implants: The most common shape, providing fullness in the upper portion of the breast. They can rotate within the breast pocket without changing the breast’s appearance.
Anatomical (Teardrop) Implants: Shaped to mimic the natural breast profile with more fullness at the bottom. These must remain in the correct position to maintain natural appearance.
Profiles
Implant profile refers to how far the implant projects from the chest wall and comes in several options:
- Low profile: Less projection, wider base
- Moderate profile: Average projection, suitable for most body types
- High profile: Maximum projection, narrower base
- Extra-high profile: Maximum projection with a narrow base, ideal for narrow chest walls
The appropriate profile depends on chest width, existing breast tissue, and desired outcome.
Texture
Smooth implants: Have a slick surface and can move naturally within the breast pocket. They typically last longer and have a lower risk of certain complications.
Textured implants: Have a rough surface designed to reduce movement and decrease the risk of capsular contracture. They adhere better to surrounding tissue but have been associated with a rare cancer called Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL).
The Surgical Procedure
Breast augmentation typically takes 1-2 hours and is usually performed as an outpatient procedure under general anesthesia. Understanding the surgical techniques can help patients better prepare for the process.
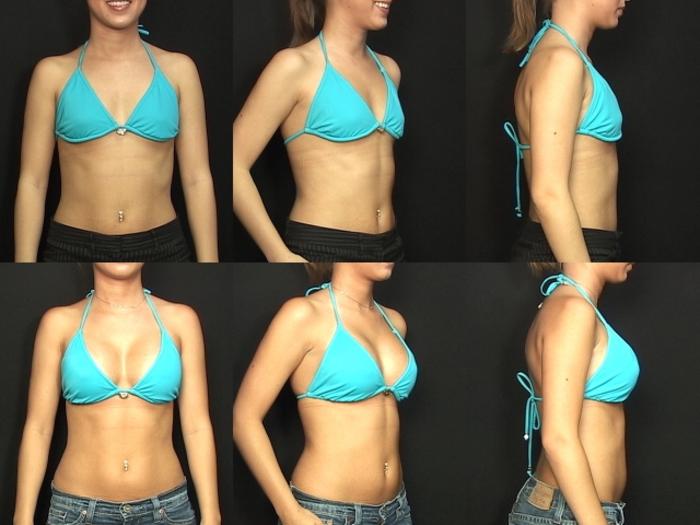
Pre-Surgical Consultation
Before surgery, patients undergo comprehensive consultations with their plastic surgeons. These appointments typically include:
- Discussion of goals and expectations
- Evaluation of breast anatomy and overall health
- Measurements and photographs for surgical planning
- Selection of implant type, size, and placement
- Review of potential risks and complications
- Preoperative medical testing as needed
Many surgeons use 3D imaging technology to simulate potential results with different implant sizes and shapes.
Incision Placement Options
Surgeons can use several incision patterns, each with specific advantages:
Inframammary: Made in the crease underneath the breast. This most common approach provides direct access to the breast pocket and leaves a scar hidden in the natural fold.
Periareolar: Made around the outer edge of the areola. This approach allows good access for precise pocket creation with a well-concealed scar, but may affect nipple sensation or breastfeeding ability.
Transaxillary: Made in the armpit. This leaves no scar on the breast but provides less direct access and visualization for the surgeon.
Transumbilical (TUBA): Made around the navel. This technique is only available for saline implants, as they are inserted empty and filled after placement.
Implant Placement
Implants can be positioned in different locations relative to the chest muscles:
Subglandular (over the muscle): Placed directly behind the breast tissue, over the pectoral muscle. This placement often involves an easier recovery but may look less natural, especially in thin women.
Submuscular (under the muscle): Placed partially or completely beneath the pectoral muscle. This provides additional tissue coverage, which can create a more natural appearance and lower risk of certain complications.
Dual-plane: A hybrid technique where the implant is partially under the muscle at the top and behind breast tissue at the bottom. This approach combines the benefits of both placements.
The Surgical Process
- Anesthesia administration (typically general anesthesia)
- Incision creation according to the predetermined pattern
- Creation of a pocket for the implant
- Insertion and positioning of the implant
- Assessment of placement and symmetry
- Closure of incisions with layered sutures
- Application of dressings and surgical bra
Some surgeons use techniques like the “no-touch” method to reduce contamination risks or place temporary drains to remove excess fluid during initial healing.
Recovery Process
Recovery from breast augmentation follows a general timeline, though individual experiences vary based on numerous factors including surgical technique, implant placement, and personal healing characteristics.
Immediate Post-Operative Period (First 24-48 Hours)
Patients typically experience:
- Grogginess from anesthesia
- Moderate pain and discomfort
- Tightness in the chest area
- Prescribed pain medication management
- Initial movement restrictions
Most patients go home the same day with detailed care instructions and a surgical bra or compression bandage.
First Week
During this critical healing period:
- Pain gradually subsides, often transitioning to soreness
- Swelling and bruising peak and begin to improve
- Limited range of motion in arms and upper body
- Sleep position limited to back with head elevated
- Avoidance of lifting anything over 5-10 pounds
- First post-operative appointment typically occurs
Most patients take at least this first week off work, longer for physically demanding jobs.
Weeks 2-4
Progress continues with:
- Significant decrease in pain and discomfort
- Reduced swelling
- Gradual return to light daily activities
- Continued wearing of surgical or support bra
- Incision sites becoming less sensitive
- Possible beginning of surgeon-recommended massage techniques
Many patients return to sedentary work after 1-2 weeks. However, strenuous activities remain restricted.
Weeks 4-6
By this stage:
- Most swelling has subsided
- Return to most normal activities, though high-impact exercise is still restricted
- Incisions have typically healed externally
- Implants begin to “settle” into their final position
- Transition from surgical bra to normal supportive bras
Patients often report feeling more comfortable with their new breast size and shape as the initial tightness resolves.
Beyond 6 Weeks
Long-term recovery includes:
- Gradual return to all exercises and activities (usually with surgeon clearance)
- Complete resolution of most swelling
- Scars beginning to fade (continuing to improve over 12-18 months)
- Implants fully settling into their permanent position (“drop and fluff”)
- Sensation returning to nipples and breast skin (may take several months to a year)
Full results are typically visible between 3-6 months after surgery when all swelling has resolved and implants have settled.
Recovery Tips and Recommendations
- Follow all surgeon instructions precisely regarding medication, activity, and wound care
- Arrange help for the first few days, especially if you have children
- Prepare a recovery area with pillows that support back sleeping
- Wear button-front tops to avoid raising arms over head
- Stay hydrated and maintain a nutritious diet to support healing
- Avoid smoking, which significantly impairs healing
- Report any unusual symptoms like excessive pain, redness, fever, or fluid discharge promptly
Potential Risks and Complications
Like all surgical procedures, breast augmentation carries risks. Being informed about potential complications helps patients make educated decisions and recognize warning signs.
Common Side Effects
These expected effects typically resolve during normal recovery:
- Temporary pain, swelling, and bruising
- Temporary changes in nipple and breast sensation
- Visible scarring at incision sites
- Firmness until tissues adapt to implants
- Asymmetry during the healing process
Surgical Complications
Less common but possible surgical risks include:
- Infection
- Bleeding or hematoma
- Poor wound healing
- Anesthesia complications
- Seroma (fluid accumulation)
- Nerve or blood vessel injury
Implant-Specific Complications
Issues related specifically to breast implants include:
Capsular contracture: Formation of tight scar tissue around the implant, causing hardening, pain, and distorted appearance. This occurs in approximately 10-15% of patients and may require surgical correction.
Implant rupture or leakage: The risk increases with implant age. Saline implants deflate noticeably, while silicone ruptures may go undetected without imaging (silent rupture).
Implant malposition: Implants can shift, rotate, or displace, resulting in asymmetry or unnatural appearance.
Rippling or wrinkling: Visible or palpable folds in the implant, more common with saline implants and in thin patients.
Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL): A rare type of non-Hodgkin’s lymphoma associated primarily with textured implants. While very uncommon, awareness of symptoms like persistent swelling or pain years after surgery is important.
Breast Implant Illness (BII): Some patients report systemic symptoms they attribute to their implants, including fatigue, joint pain, cognitive issues, and autoimmune-like symptoms. Research continues into this controversial condition.
Long-Term Considerations
Issues that may develop or require attention over time:
- Implants are not lifetime devices; replacement surgery may be needed
- Changes in breast appearance with aging, pregnancy, or weight fluctuations
- Need for additional procedures like breast lift if natural sagging occurs
- Interference with mammography (special displacement techniques may be needed)
- Impact on breastfeeding (most women can breastfeed but some experience difficulties)
The FDA recommends MRI screening three years after receiving silicone implants and every two years thereafter to check for silent ruptures.
Cost Factors and Financing
The cost of breast augmentation varies significantly based on multiple factors. Understanding the complete financial picture helps patients plan appropriately.
Average Cost Ranges
In the United States, breast augmentation typically costs between $5,000 and $10,000. This wide range reflects variations in:
- Geographic location (higher in major metropolitan areas)
- Surgeon experience and reputation
- Implant type (silicone generally costs more than saline)
- Facility fees (hospital vs. outpatient surgical center)
- Anesthesia fees
What’s Included in Quoted Prices
When researching costs, patients should verify what the quoted price includes:
- Pre-operative consultations
- Surgeon’s fee
- Anesthesia fees
- Operating room facilities
- Implant cost
- Post-operative visits
- Surgical garments
Some practices quote comprehensive packages while others itemize costs. Verify whether revision surgery costs are addressed in the event of complications.
Insurance Considerations
Purely cosmetic breast augmentation is rarely covered by health insurance. However, reconstructive breast surgery following mastectomy is typically covered under federal law. In certain cases, insurance may cover:
- Breast reconstruction after cancer treatment
- Correction of congenital deformities like severe asymmetry or tuberous breasts
- Revision of complications from prior medically necessary breast surgery
Patients should consult their insurance providers about specific coverage policies and obtain pre-authorization when applicable.
Financing Options
Many patients finance their breast augmentation through various methods:
- Medical credit cards (CareCredit, Alphaeon) specifically designed for healthcare expenses
- In-house payment plans offered by surgical practices
- Personal loans from banks or credit unions
- Healthcare installment loans from specialized finance companies
- Health savings accounts (HSAs) or flexible spending accounts (FSAs) for certain reconstructive procedures
When considering financing, patients should carefully review interest rates, payment terms, and total cost over time.
Additional Cost Considerations
Beyond the initial surgery, patients should budget for:
- Time off work during recovery
- New bras and clothing
- Prescription medications
- Possible future imaging (MRIs for silicone implants)
- Long-term maintenance or replacement surgery (implants are not lifetime devices)
Experts recommend planning for potential implant replacement every 10-15 years, though many implants last longer without issues.
The Consultation Process
A thorough consultation helps assess both technical skill and personal compatibility. Look for a surgeon who:
- Listens carefully to your goals and concerns
- Provides comprehensive education about options
- Shows realistic before-and-after results
- Discusses limitations and potential complications honestly
- Answers questions clearly without pressure
- Performs a detailed physical assessment
- Offers multiple options tailored to your anatomy
Many patients benefit from consulting multiple surgeons before making a decision.
Facility Accreditation
Surgery should be performed in an accredited facility with proper safety standards:
- Accreditation by organizations like the American Association for Accreditation of Ambulatory Surgery Facilities (AAAASF)
- Properly trained staff including certified anesthesia providers
- Emergency protocols and equipment
- Hospital transfer arrangements if needed
Facilities should maintain strict infection control and patient safety standards.
Preparing for Surgery
Proper preparation improves both safety and recovery experience. Most surgeons provide detailed pre-operative instructions, which typically include:
Medical Preparations
- Laboratory testing: Blood work, EKG, or other tests as recommended
- Medication adjustments: Stopping blood thinners, certain supplements, and anti-inflammatory drugs
- Baseline mammogram: Recommended for patients over 40 or with family history
- Medical clearance: From primary care physician if you have health conditions
Lifestyle Adjustments
- Smoking cessation: At least 4-6 weeks before surgery to improve healing
- Alcohol reduction: Minimizing consumption for at least a week before surgery
- Healthy diet: Focusing on protein and nutrients that support healing
- Hydration: Maintaining good fluid intake
Practical Preparations
- Arranging help: Transportation home and assistance for the first 24-48 hours
- Work arrangements: Planning appropriate time off
- Home setup: Preparing a comfortable recovery area with everything within easy reach
- Meal preparation: Preparing easy meals in advance
- Recovery supplies: Purchasing front-closing shirts, extra pillows, prescribed medications, ice packs, etc.
Mental and Emotional Preparation
- Setting realistic expectations about results and recovery timeline
- Understanding that final results take months to develop
- Addressing any anxiety through thorough research and communication with your surgeon
- Preparing for possible “post-surgical blues” during the initial recovery period
Conclusion
Breast augmentation can significantly enhance appearance and confidence when performed by qualified surgeons on appropriate candidates with realistic expectations. The procedure has evolved considerably over decades, with improvements in implant technology, surgical techniques, and safety protocols.
Success depends on thorough research, careful surgeon selection, and understanding both the benefits and limitations of the procedure. While breast augmentation can create dramatic improvements in breast size and shape, it requires commitment to follow-up care and acceptance that additional procedures may be necessary over time.
For those considering breast augmentation, a consultation with a board-certified plastic surgeon provides the opportunity to discuss individual goals, assess candidacy, and develop a personalized surgical plan. With proper planning and care, breast augmentation can provide satisfying, long-lasting results that align with personal aesthetic goals.